
While we enjoy a welcome break in summer temperatures after July’s endurance test, it’s easier to think again about how planning for ways to make our lives in the city cooler and safer in the future.
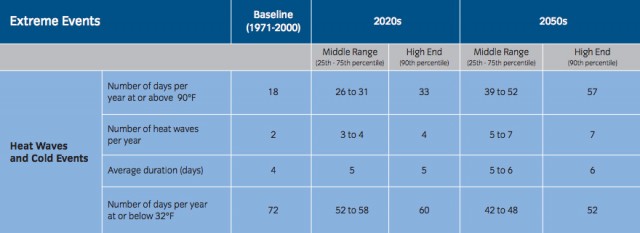
The environment and human health are linked: when the environment is stressed, health can be compromised in a number of ways. The Healthcare Section of this summer’s SIRR report on resiliency after Sandy states that storm surge and heat waves will be the primary climate risks facing the healthcare system in the coming years. These trends are not unique to New York, and the number of days above 90-degrees per year is projected to rise.
Additionally, the urban heat island effect keeps temperatures in densely populated areas higher than surrounding areas. Extreme events like Hurricane Sandy that lead to disruptions in the health care system can have dramatic consequences for the many New Yorkers who depend on it. (Consider the combined effect of a storm that knocks out power, which is followed by a heat wave. That could leave New York’s most vulnerable, the elderly, stranded in high rise buildings without power, water, or relief. Both events happened in 2012, but fortunately were separated, and the storm, Sandy, came in the cooler months.)
So what can be done to improve and maintain the level of care for New Yorkers? We were very glad to see concrete and detailed suggestions in the SIRR. Proposals for full resilience and crisis care include:
1. Improve the design and construction of new hospitals
2. Require the retrofitting of existing hospitals in the 500-year floodplain
3. Support the Health and Hospitals Corporation (HHC) effort to protect public hospital emergency departments from flooding
4. Improve the design and construction of new nursing homes and adult care facilities
5. Require the retrofitting of existing nursing homes in the 100-year floodplain
6. Require the retrofitting of existing adult care facilities in the 100-year floodplain
7. Support nursing homes and adult care facilities with mitigation grants and loans (The report recounts that during Sandy 61 nursing homes and adult care facilities were in areas impacted by power outages and/or flooding and 28 facilities [were] evacuated under emergency conditions, causing additional stress)
8. Increase the air conditioning capacity of nursing homes and adult care facilities
9. Harden primary care and mental health clinics
10. Improve power resiliency for pharmacies and other medical facilities
11. Encourage telecommunications resiliency
12. Encourage electronic health record-keeping
13. To ensure longer-term population health, in addition to these measures, the focus needs to shift from treatment to prevention. Developing community-based health and resource centers can serve the dual role of informing residents and providing care in a trusted environment during times of crisis. A number of future health risks (from heat increases and demographic/population shifts where socioeconomic status and vulnerability for health related morbidity and mortality are correlated) can be addressed head-on with information campaigns.
Some examples include the need for hydration when it’s hot, establishing cooling centers (that provide air conditioning), offering free rides to these centers, and also offering preventive screenings for high risk individuals to forestall their need for hospital services. Investing in disease prevention can and will reduce city expenditures on treatment, which is a financial burden to the entire population.
14. There were at least two additional, forward-thinking measures not covered in the report but highlighted by healthcare professionals attending the Municipal Art Society SIRR event in response to the report’s release in June. One point that could not be stressed enough was a dire need for strengthening communication between the city’s healthcare facilities, especially regarding emergency readiness. For example, during an emergency such as a hurricane, if a hospital further away from a hard-hit zone has beds, mobile staff, or other resources available and can help out in concrete ways, lives, resources, and time can be saved if communication systems are in place to mobilize healthcare resources to the fullest extent.
Another suggestion was that in the case of extreme weather, emergency prescription capabilities should exist, so that patients in critical need of medication are able to access their records and medication even if they have been relocated suddenly, or if their primary care provider or pharmacy/pharmacist are unreachable or if facilities have been destroyed.
The impacts of the changing climate will be felt first by those most vulnerable (i.e. the poorest and those without social networks), so it is essential to develop systems of protection and support. The resilience measures for infrastructure and people proposed in and after the report can become part of a greater effort to improve the overall health of New York.
Image: NYC.gov. There are 1,985 water fountains in NYC parks!